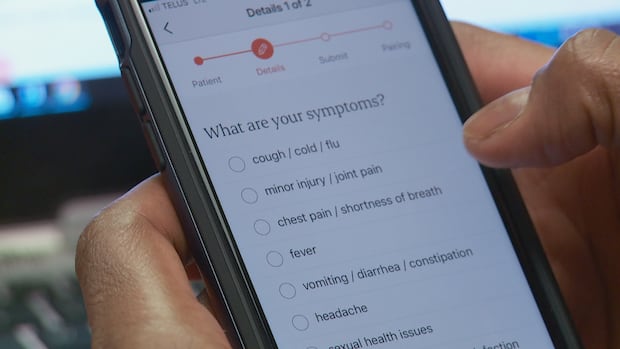
For several months, Alyssa Greene has been without a doctor, so when she needed a prescription refill last month, she turned to eVisit, a virtual primary care service. The process wasn’t as easy as she expected. Greene says she logged onto the app at noon and waited for three hours before receiving a notification saying, “There’s no one here to help you today.” The next day, Greene tried again, logging on around 10 a.m. and getting paired with a nurse practitioner shortly after 2 p.m. Greene considers her experience positive once she could speak with the nurse practitioner, but thinks virtual appointments are not an ideal way for those without family doctors to access primary care.The eVisit service is delivered free through an app called Maple to New Brunswick residents without family doctors and to people who can’t access their providers in a timely manner. The service is open from 8 a.m. to 8 p.m. daily and is for non-emergency medical concerns. Greene said virtual care can feel impersonal because there isn’t an established relationship with the provider and it’s done over the phone. Trust with a provider is important, much like it is with a car mechanic, she said.“Usually, you’ve developed a relationship with the person that you take your car into regularly and get it maintained. Why would you do any different with your body?”Greene worries that virtual care may be her only source of primary care for a while. “There has to be something else, otherwise people are just going to keep going to emergency rooms and filling that up with non-emergent cases because you have no other choice.”Stéphane Robichaud, CEO of the New Brunswick Health Council, says virtual care is growing in popularity. (Katelin Belliveau/CBC)Stéphane Robichaud, CEO of the New Brunswick Health Council, said Greene’s concerns are not unique. Long wait times on the eVisit app are caused by the service growing in popularity and New Brunswick’s growing population, when resources in the province are limited.A growing demandIn the 2024-25 fiscal year, the Department of Health reported the number of eVisit users grew by 38 per cent over the previous year, and the number of virtual appointments increased by almost 24 per cent.Nancy Theriault, a virtual care nurse practitioner, has felt the effects of the growing demand first-hand. WATCH | Ensuring people can ‘access a form of care that works for them’ :Health researcher points to access problems related to virtual careThe New Brunswick Department of Health says eVisit users increased by almost 40 per cent in the 2024-25 fiscal year. She said that when she first started in this work, she was putting in hours of overtime.“I would put my son to bed and go back online and work for another few hours before I went to bed, I did that for a long time.”But she realized she couldn’t address the “mountain” of people needing care on her own.“We can’t see everybody because the demand is so high,” she said. “When we log off, it’s to protect ourselves so that we will be there tomorrow.” Sharon Hamilton, president of Nurse Practitioners of New Brunswick, said that on top of working full time, many nurse practitioners work part time on virtual care platforms.Sharon Hamilton, president of Nurse Practitioners of New Brunswick, says virtual care isn’t a long-term solution to the shortage of primary care providers. (Submitted by Sharon Hamilton)She doesn’t believe virtual care is sustainable as a long-term solution for the shortage of primary care providers.Hamilton said it’s not good practice to “be renewing somebody’s prescriptions without them being seen in person” as they often “need to be changed, they need adjustment.”No continuity of careHamilton said the service could be improved if providers were able to follow up with patients on the app. “They get lost in the system, they start again, they call back and well, they might get another provider so there’s no continuity of care,” Hamilton said. Robichaud said studies done by the New Brunswick Health Council have found patients are concerned about followup and continuity of care.“For an important proportion of our population, a lot of their issues are interrelated,” he said. It’s a problem that “the provider on the other side doesn’t have any information at his disposal.”Katharine Dunbar, a health equity researcher and professor at Mount Allison University, points to another challenge when it comes to virtual care — access.Issues include “gaps in digital literacy, the gaps in broadband internet,” she said. “There are certainly rural areas where internet access is an ongoing issue, this is going to limit people’s abilities to access digital or virtual care.”Dunbar said financial resources can also cause difficulty, especially when people don’t have many digital devices in their household. Katharine Dunbar, a health studies professor at Mount Allison University, says the biggest issues with virtual care are related to access. (Submitted by Katharine Dunbar)“Maybe you don’t have a private space where you can have a medical appointment without other people hearing your conversation,” she said.“These can all be factors where people might otherwise benefit from virtual care but are unable to as a result of the material conditions in which they live.”A system that works togetherRobichaud hopes that eventually, virtual care will be a small part of primary care, used only when it meets the needs and makes the most sense for the patient. He said virtual care isn’t currently integrated into the health care system, but he hopes New Brunswick will one day get to a point where it is “just one of the different ways that they’re offering better care to their patients.”WATCH | Ensuring people can ‘access a form of care that works for them’ :Health researcher points to access problems related to virtual careThe New Brunswick Department of Health says eVisit users increased by almost 40 per cent in the 2024-25 fiscal year. Theriault agreed that a full integration of health services would improve care. Providers working through eVisit may have to make determinations about a patient’s health and review their medical history “kind of blind,” she said. “Everything that happens on our platform is seen on our platform only.”5-year plan calls connected care a priorityNew Brunswick’s five-year health-care plan, announced earlier in October, lists care through integrated digital systems as one of six priorities. The report says the goal is for New Brunswickers to “receive co-ordinated, timely and personalized care through a fully integrated digital health ecosystem” by the fall of 2026. However, Health Minister John Dornan said the immediate priority for improving the system is to ensure every New Brunswicker has a family doctor. His government hopes to accomplish that goal by opening 30 collaborative care clinics by 2028. Premier Susan Holt promised to establish 10 of those clinics by the end of this year, and six have already been opened. Health Department spokesperson Meghan Cumby told CBC News in July that New Brunswick’s contract with eVisit expires on April 1, 2026, and didn’t confirm whether it would be continued.
Growing use of virtual care in N.B. comes with its own access problems